Diffusion cell apparatus is used to measure in vitro release of drugs from creams, ointments, oils, and gels.
Conduct Science’s diffusion cell apparatus offers an objective assessment of the velocity and depth of drug penetration through the skin of living animals in a specified solvent. This apparatus plays a pivotal role in scientifically screening effective drugs with transdermal absorption capabilities. Recognized internationally, it stands as a standard method for detecting and evaluating drug transdermal release, contributing significantly to the advancement of pharmaceutical research and development.
ConductScience offers the Diffusion Cell Apparatus.
Images are illustrative.
$2,800.00
10% off with your subscription Membership

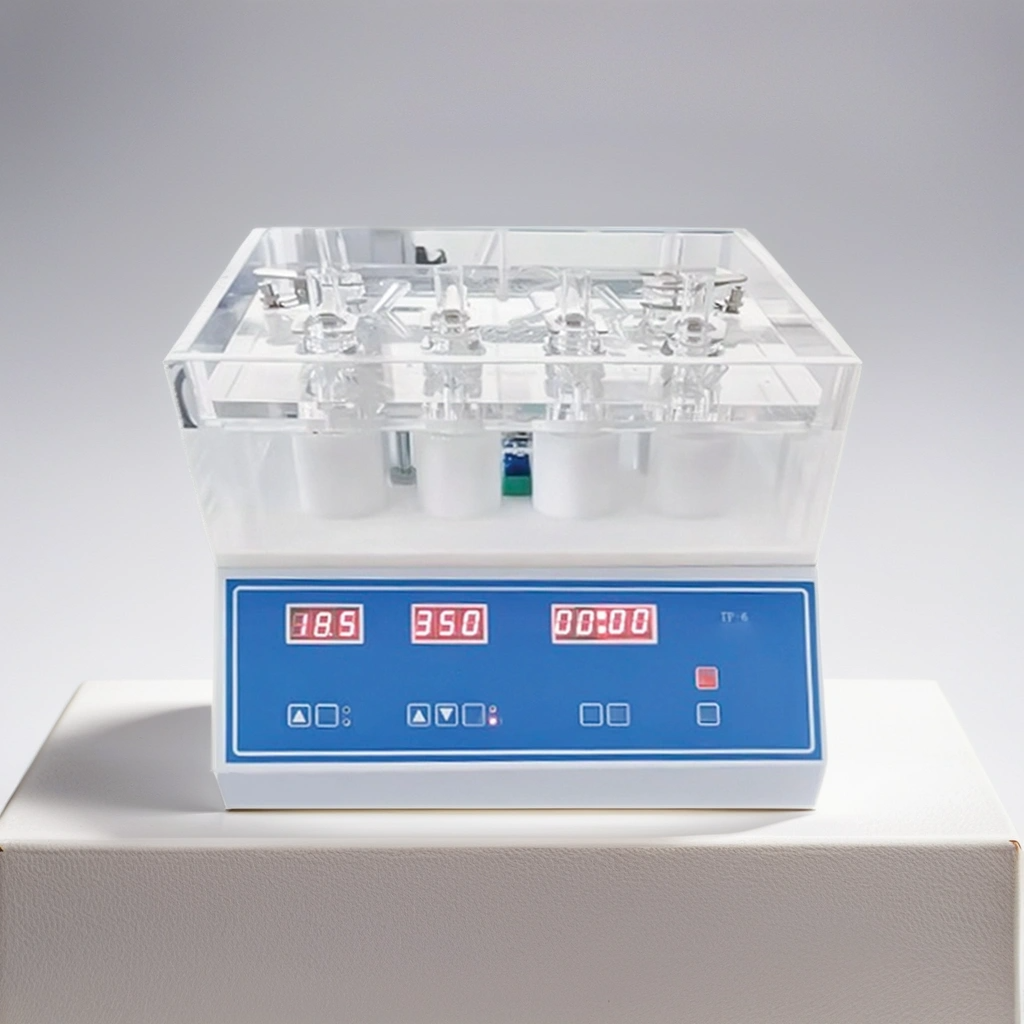
Conduct Science’s diffusion cell apparatus offers six stirring with six transdermeal cups at 15ml cell capacity. It comes with a digital RPM indicator and speed controller, a water level indicator, and a digital temperature controller. The cell holders contain diffusion cells with stirring bars. The apparatus provides constant stirring to the solutions. It comprises a water heater that helps in attaining the desired temperature. The water circulation system is also provided with a water level sensor that protects the heating element from damage. A magnetic induction knob aids the heavy-duty stirrers to offer constant and non-stop stirring. The stirring range lies between 200 and 800rpm. Moreover, the stainless-steel body of the cell apparatus makes it corrosion-free. Sheet membrane is required to be cut to size for each diffusion cell.
Six Stirrings
Water Heater
Digital RPM Indicator
Speed Controler
Water Level Indicator
Six Transdermal Cups
Cell Holders: Diffusion Cells + Stirring Bars
Constant Stirring of Solutions
Stainless-steel body of cell apparatus
Digital Temperature Controller
The diffusion cell apparatus is used to measure in vitro release of drugs from creams, ointments, oils, and gels. Diffusion is the random movement of molecules across the concentration gradient, i.e., from high concentration to low concentration. In vitro diffusion is the passive diffusion of a solution molecular species from a donor chamber through a membrane into a ‘receptor fluid’ present in the recipient compartment.
The molecular species passing/diffusing through the membrane is called ‘permeant.’ ‘Permeation’ is defined as “the movement of the permeant through the tissue/membrane that incorporates the first membrane and then diffuses through the membrane.”
Flux is defined as the amount of permeant crossing through per unit area of the membrane into the circulating system per unit time. In in vitro diffusion, the circulating system is referred to as the ‘system’ and expressed in mass, area, and time.
The amount of molecules passing through the membrane in the given time is known as accumulation and is defined in mass and area.
Diffusivity is a characteristic of permeant that measures its ease of penetration through a particular membrane and is expressed in area/time.
Permeability coefficient is described as the ‘rate of penetration of the permeant per unit concentration,’ expressed in units of distance/time.
Any permeant that permeates through a membrane diffuses into the receptor fluid and reaches a steady state of diffusion takes some time. This time is the ‘lag time.’ The permeation rate across the membrane rises in the lag time. Once the sample reaches a steady state, the movement of permeant through the membrane becomes consistent. The attainment of steady-state depends on various factors, including membrane/tissue permeability, compound properties, and the receptor fluid flow rate.
The permeability barrier is a lipid barrier for human cells that depends on lipid type and organization. It should be noted that the permeability of tissue is not related to its thickness. For instance, different permeants exhibit different permeability over different sites on human skin.
The working of diffusion cell apparatus or Franz cell is based on ‘in vitro diffusion.’ It consists of two chambers, a donor compartment and a receptor compartment, separated by a membrane. The product to be tested is introduced through the donor compartment (the top chamber). The bottom chamber or the receptor compartment contains fluids from which samples to be analyzed are extracted at regular intervals. The sample collected determines the amount of “active” that permeates through the membrane at point time. The cell temperature constantly remains at 37oC. The receptor compartment of a diffusion cell or Franz cell has a fixed volume, and it allows the stirring of both receptor and donor chambers (Kelin et al., 2018).
A diffusion cell apparatus helps to evaluate compound uptake into the membrane and determines tissue/membrane permeability, concentration in the receptor compartment, and flux. When working with a highly permeable compound and a large receptor compartment, the reduction in the gradient builds up the compound in the receptor chamber. On the other hand, if the receptor chamber is small, the concentration gradient is reduced due to compound buildup. The reduction in concentration gradient ultimately slows down the compound flux resulting in non-sink conditions. However, if the compound has low permeability, the detection of the compound in a large volume receptor chamber can be problematic.
Various types of membranes can be used for diffusion experiments. Some of these are given below:
While selecting a suitable membrane, one must consider its source, integrity, time of excision, and shelf life. If it is obtained from an animal source, the scientist must know the health and age of the animal, and if the source is human, the researcher must consider the race, age, and gender of the human. If the permeability of the membrane/tissue is altered, it may affect the results of your experiment. Therefore, the experimenter must know beforehand whether the membrane was exposed to any chemicals. Skin tissue, however, may be refrigerated and used later without a change in permeability.
The donor compound can be prepared as liquid, gel, suspension, ointment, lotion, powder, or adhesive patches. One can determine permeant behavior and characteristics based on concentration and permeability.
The permeant concentration depends on the aim of the study. An infinite dose is when the permeant does not deplete from the donor compound throughout the experiment and is used to test fundamental permeation behavior in the presence of permeability enhancers. On the contrary, a finite dose relates to the permeant amount that would be practical in actual usage, for example, a specific amount of drug to be administered to a patient. It aims to determine the amount of permeant required to be incorporated in a vehicle that will deliver the required amount of drug to the patient. Alternatively, the application of a compound that will temporarily remain on the tissue can be mimicked. In this case, the permeant is applied to the membrane for a short time and then removed. The researcher should then collect the samples for a given length of time following permeation.
The vehicle is the medium in which the permeant of interest is incorporated. Vehicle formulation is the “dose to be administered without the drug or active pharmaceutical agent (API).” Aqueous solutions and phosphate buffers serve as excellent vehicles for getting basic permeation data. Lipophilic compounds, however, have low solubility in aqueous solutions. Therefore, vehicles like water, alcohol, or propylene glycol should be used while working with them. Inert materials may alter the flux of compounds.
Moreover, the potency of enhancers may be altered by the nature of the vehicle. A selection buffer controls the degree of ionization; therefore, adjusting pH can completely dissociate the permeant into ions. Furthermore, vehicle components may also be modified by thermodynamic activity.
Spectroscopy and chromatography techniques are used for permeant detection.
A group of five to six replicate doses should be administered to avoid errors resulting from the biological variability of skin. A minimum of three parallel cells should be used for testing each formulation.
The receptor solution is selected based on the nature of the permeant. An ideal receptor compound should mimic in vivo situations. The accumulation in the receptor compartment is minimized by using flow-thru systems, and aqueous receptor fluid is sufficient for this purpose. On the other hand, it raises a concern for static cells where the permeant is not continually cleared. The solubility of the compound is a major concern in this regard. It should be such that it is in its desired form in the donor media and delivered in a certain amount to the receptor compound. Hydrophilic and lipophilic permeants show the best results with the aqueous receptors.
Similarly, PBS is used for ionizable permeants. If the permeant is un-ionizable, a solubilizer should be added to the receptor compound. Moreover, permeants with low aqueous solubility, like lipophilic permeants, require additional solubilizing agents such as surfactants or organic solvents. However, these agents might alter the membrane permeability and damage or alter the tissue/membrane. Therefore, one should use the minimum possible amount of these agents.
The method of sampling depends on your research question. One can measure the amount of compound passing through the membrane at short intervals or the total amount that passes over a long-time duration. One can also determine flux, permeability constant (Kp), accumulation, etc., using a diffusion cell apparatus.
The researchers can use radiolabeled or unlabeled compounds for measuring flux and permeability. The results are reported as one of the two types of accumulation:
Radiolabeled compounds can be detected in very small amounts in large volumes of receptor media; however, the results are accurate and robust for such compounds. On the other hand, non-radiolabeled compounds used in permeability research can be detected using HPLC and ELISA methods.
Calculating flux and Permeability Constant
Flux is the amount of permeant passing through the membrane in unit time. It is measured in ‘Joules’ (J), and its formula is given by: J=Q/ (A x t). In the given formula, Q is the amount of permeant crossing the membrane in time t, and A is the membrane area usually given in cm2.
Steady State Flux is the amount of permeant crossing the membrane at a constant rate. This state is achieved after the lag phase as the amount of permeant continues to increase. When you measure the amount at regular short intervals at this stage, no significant difference in the values is observed. The units of steady-state flux (Jss) are quantity/(cm2*h). the formula for calculating steady-state flux is J = dQ/dt*A, where it is the permeation time, and A is the membrane area in cm2.
Permeability constant (Kp) can be calculated by using the formula Kp= Q/ [A*t*(Co-Ci)]. It is measured when an infinite dose of permeant is applied to the membrane. In the given formula, Q is the quantity of the permeant passing through the membrane in time t, A is the area of the membrane (cm2), Co is the concentration of the compound on the outer side (donor chamber), and Ci is the compound concentration on the inner side (receptor chamber).
The apparent permeability of the solution can be calculated by normalizing ‘J’ over drug concentration in the donor compartment Co, i.e., Papp = J/ Co.
In-vitro Release Testing
In vitro release testing (IVRT) employs diffusion cell apparatus to evaluate topical dosage form’s performance and determine the physiochemical properties of a product. Kelin et al. (2018) examined the critical parameters of diffusion cell apparatus and developed methods using this apparatus. IVRT has been used for the past 50 years to understand the release rates of products like hydrocortisone and betamethasone dipropionate. It allows the optimization of a drug formulation to make it ideal for in vivo use. This method also helps establish novel drugs’ sameness by making minor changes in drug formulations during clinical testing. These minor changes ensure the sameness of the drug between clinical development stages. They stated that VDC (vertical diffusion cell) method could be validated by assessing attributes like drug solubility and stability in receptor media, binding the drug to the membrane, release rates precision, discrimination sensitivity, selectivity, and specificity, the sturdiness concerning critical parameters, and many others. Moreover, several parameters (like temperature, diffusion cell dimensions, sampling intervals, receptor fluid, membrane, and the amount of the permeant applied to the membrane) are tightly controlled to optimize the permeation experiments using VDC (Klein et al., 2018).
Pre-formulation Characterization of Semi-Solid Dosage Forms
Salamanca et al. (2018) evaluated the ketoprofen (KTP) releasing profiles of two drug formulations, i.e., a gel and a suspension. Ketoprofen is a widely used drug for treating rheumatoid arthritis, spondylitis, osteoarthritis, and gout. The researchers prepared KTP suspension by mixing 12.5g of ketoprofen with 2 ml of glycerin and 500ml of ultra-pure water and used 2.5g of sodium alginate as a suspensor agent. On the contrary, they similarly prepared KTP gel with an additional 2.5g of calcium chloride. The experiment was conducted in three individual Franz cells with 125ml volume of the acceptor compartment and membrane area of 2.5cm2. The amount of permeant in the donor chamber was set at 5g. the samples were stirred at a speed of 480rpm for 24 hours. They used triplicates of each sample and maintained the temperature throughout the experiment at 37oC. Samples were evaluated at regular short intervals, and the scientists measured their releasing efficiency in terms of mass flux. Two aqueous media were used as acceptor phases imitating the physiological conditions corresponding to buffers with pH 5.6 and 7.14 at 0.15M.
Furthermore, two types of membranes were used, i.e., regenerated cellulose membrane and a transdermal diffusion test. Mass flux was calculated using the formula, and kinetic study of ketoprofen permeation was done using statistics. The researchers concluded that the gel formulation had higher permeation efficiencies as compared to the suspension. They also reported that evaluating the performance of pharmaceutical products at the pre-formulation stage becomes easier if one uses artificially engineered membranes.
Evaluation of cinnamon oil and chlorhexidine permeation through C. Albicans biofilm
Satthanakul et al. (2020) presented an in vitro method to analyze the permeation of cinnamon oil and chlorhexidine (CHX) through Candida albicans biofilm using diffusion cell apparatus. C. Albicans biofilms contain extracellular polymeric substances (EPS) that act as a barrier to antifungal agents like the mentioned products and prevent them from reaching the target site of the yeast cells. They prepared cinnamon oil and CHX solutions and grew C. Albicans biofilms on membrane filters by inoculating 50µL of C. Albicans on the UV-exposed sterilized filters. They allowed different combinations of CHX and cinnamon oil to pass through the biofilm. To achieve this, they filled the Franz cell with 5.3ml of the sample solution. The sample solution contained 0.5% w/v CHX and 8µL/ml cinnamon oil or 0.2% w/v CHX and 8µl/ml of cinnamon oil. The researchers maintained the volume by adding the solution to the sample port. The sample was stirred at 50rpm for homogenization, and the temperature was maintained at 37oC to mimic the oral cavity environment. The C. Albicans biofilm cultivated at 25mm membrane filters was mounted into a sample holder, and smaller-sized filters were placed on the fixed biofilm. The paper disks moistened with 10µl distilled water were placed on the membrane filters to prevent capillary action. The sample holder was covered with the cap, and the Franz cell was assembled. The experimenters set the temperature at 37oC via a temperature controller and collected paper disks at regular intervals. The disks were then placed on Sabouraud dextrose plates containing C. Albicans. Zones of inhibition were measured after 48 hours of incubation at 37oC. They compared these inhibition zones with the zones formed by cellulose membrane filters lacking biofilms. The sessile biofilms were tested for viability, and the results were subjected to statistical analysis. They concluded that sessile C. Albicans biofilms tested with 0.5% w/v CHX and 8µl/ml of cinnamon oil resulted in a “4 hours log reduction”.
Biomimetic Artificial Membrane Permeability Assay
Permeability of oral drugs through the lipid bilayer of the intestinal epithelial cells is an important parameter to measure the extent of drug absorption. Teixeira et al. (2020) validated a biomimetic artificial membrane permeability assay to assess the permeation profile of six drugs, namely “acyclovir, cimetidine, diclofenac, ibuprofen, piroxicam, and trimethoprim,” along with eight model drugs from the Biopharmaceutic Classification System (BCS) using a diffusion cell apparatus. They impregnated the membrane supported with a solution containing a mixture of phospholipids and weighed it on a microanalytical scale. These impregnated membranes were then refrigerated to protect them. They positioned the impregnated membranes between the donor and the recipient compartments for permeation studies, each containing PBS, and stirred the receptor media at 500rpm.
Moreover, they maintained the temperature at 37oC and added triplicates of each drug in the donor compartment. The donor compartment contained a fixed concentration of the fluid, i.e., 10mg/ml and 1ml of saturated drug solution, and was capped to avoid evaporation. They ran the experiment under infinite dose conditions except for these drugs: caffeine, atenolol, metoprolol, naproxen, propranolol, and ranitidine. Drug solubility for each compound was measured. Then the researchers did permeability calculations using appropriate formulas. They classified 10 out of 17 drugs as low permeability drugs, and out of these 10, the permeability of only three drugs was underestimated as per BCS.
Ease of Reproducibility. Limited tissue handling. Minimal Sample Collection Requirements.
Low Drug Sample Requirement. Versatility in Permeation Studies:is well-suited for various permeation studies, allowing researchers to investigate the diffusion of substances across membranes under controlled conditions.
Limited Sensitivity with Radiolabeled Compounds. Challenges in Handling Radiolabeled Substances.
Klein, R. R., Heckart, J. L., & Thakker, K. D. (2018). In vitro release testing methodology and variability with the vertical diffusion cell (VDC). Dissolution Technol, 25(3), 52-61.
Salamanca, C. H., Barrera-Ocampo, A., Lasso, J. C., Camacho, N., & Yarce, C. J. (2018). Franz diffusion cell approach for pre-formulation characterisation of ketoprofen semi-solid dosage forms. Pharmaceutics, 10(3), 148.
Teixeira, L. de Souza., Vila Chagas, T., Alonso, A., Gonzalez-Alvarez, I., Bermejo, M., Polli, J., & Rezende, K. R. (2020). Biomimetic Artificial Membrane Permeability Assay over Franz Cell Apparatus Using BCS Model Drugs. Pharmaceutics, 12(10), 988.
Satthanakul, P., Taweechaisupapong, S., Luengpailin, S., & Khunkitti, W. (2020). In vitro method for studying the penetration of cinnamon oil and chlorhexidine through Candida albicans biofilm using Franz diffusion apparatus. Songklanakarin Journal of Science & Technology, 42(2).1
| Weight | 20 kg |
|---|---|
| Dimensions | 700 × 700 × 600 cm |
| Stirrer | 6 Stage Stirring |
| Transdermal Cup | 6pcs |
| Capacity of Cell | 15 ml Vertical Cells (Standard), 10 ml Vertical Cell, 5 ml Horizontal Cells (optional) |
| Temperature Control Range | 30-40℃ |
| Temperature Control Precision | ±0.1℃ |
| Stirring Speed Range | 100-800r/min |
| Speed Precision | ± 5% |
| Power Supply | Standard: 220V, 50/60Hz, Optional: 110V, 50/60Hz |
| Power | 360W |
| Dimensions | 42cm x 42cm x 38cm |
| Gross Weight | 12kg |
You must be logged in to post a review.
DISCLAIMER: ConductScience and affiliate products are NOT designed for human consumption, testing, or clinical utilization. They are designed for pre-clinical utilization only. Customers purchasing apparatus for the purposes of scientific research or veterinary care affirm adherence to applicable regulatory bodies for the country in which their research or care is conducted.

Reviews
There are no reviews yet.